‘It is the end … but the moment has been prepared for.’
The Gallifrey Institute for Learning has no affiliation with the BBC or actual Gallifrey. The courses provided by the Gallifrey Institute for Learning are intended for educational purposes only. We do not accept any responsibility for information from the programmes being used to harm any Gallifreyans, no matter how irritating or destructive they might be.
Nothing in this guide constitutes professional medical advice - always seek your human advice from a healthcare provider, and always seek your Gallifreyan advice from a hospitaller on Gallifrey.
The Institute welcomes any comments, suggestions, questions, corrections, contributions, one-liners, small essays, amusing gifs, or whatever takes your fancy. Please contact us via message or our ask on Tumblr or via email using the envelope icon above.
Everything in this guide is free to be challenged and changed. If you have any information, please have a source/reference so it can be verified.
If you are enjoying the course and are able to do so, please consider buying us a coffee or tipping Tumblr to sustain our tired human writer with caffeine.
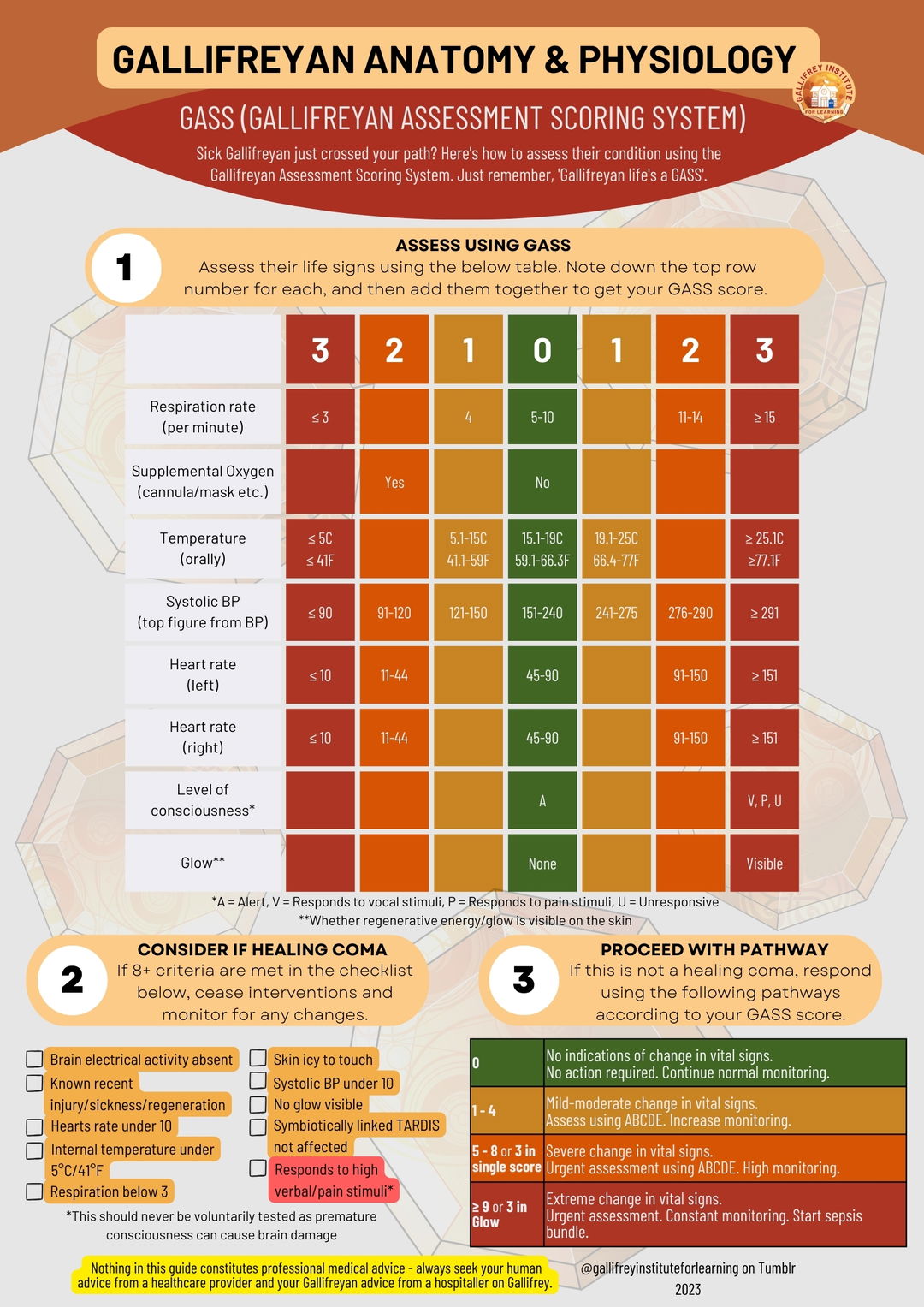
Any good human healthcare provider will start any medical encounter with a vital sign check (aka observations). Unfortunately, Gallifreyan observations will greatly vary from human norms, leading to some very catastrophic misunderstandings.
- Blood pressure: The normal BP of a Gallifreyan will be mistaken by human medics for hypertension. Any human medications used will cause hypotension.
- Heartsrate: Normal heartsrate will be mistaken for tachycardia. Any medications used will cause bradycardia, leading to oxygen deprivation, fainting, and cardiac arrest of the heart(s).
- Respiration rate: Anything from 12-20 rpm is considered normal in humans. Any supplemental oxygen given won't be necessary in Gallifreyans, and human medics may miss a serious problem.
- Temperature: This is extremely low compared to humans. Attempts to raise the core temperature will result in hyperpyrexia, and if prolonged enough, heatstroke, coma, and death.
- Oxygen Saturation: Oxygen in Gallifreyans does not travel in the blood and therefore normal human O2 monitors will always error code or show 0%.
- Blood glucose: Normal Gallifreyan ranges would be considered an emergency in humans, but any attempt to control this will result in ketotic hypoglycaemia.
Immediate response
- Ensure own personal safety by checking for environmental hazards such as stray Daleks.
- Observe patient briefly to see if they appear unwell.
- Try to verbally stimulate them with, 'how are you?' and following with shaking the shoulder and saying, 'are you all right?'
Is it a cardiac arrest?
If unconscious, check for normal breathing and check for a pulse. If not present, start CPR on both hearts. If this isn't a cardiac arrest of both hearts, start ABCDE.
⚠️
Check before performing CPR that this is not a healing coma. A healing coma can be identified by minimal respiration, a very low skin temperature, and heartsbeat only accessible by a stethoscope, of under 10 beats per minute. They will not respond to vocal or pain stimuli and be pretty annoyed if your break their ribs doing CPR when they wake up.
Proceed with ABCDE assessment
Head through the below list one by one, checking for each issue raised and dealing with them as they're identified. Reassess after every intervention.
🌱
The following contains links to medical procedures on dummies or actors. Viewing them is entirely optional.
📘
Can the patient talk? If yes, move on to Breathing as their airway is clear.
Check for airway compromise.
- Check for any visually obvious obstructions in the mouth such as a foreign object.
- Check for any fluids such as blood/vomit - possibly indicative of trauma.
- Check for swelling - possibly indicative of an infection or anaphylaxis.
- Check for any masses - possibly indicative of a tumour.
Observe their breathing.
- Is it noisy/interrupted/raspy/stilted? Is their chest raising and falling in a 'see-saw' like motion? - They may have a partially obstructed airway.
- Are they not breathing at all? - They may have a completely obstructed airway.
Note their skin colour.
- Are their skin or their lips pale/purple? - They may have a completely obstructed airway.
⚠️
If they are not breathing and feel cold but are maintaining normal lip/skin colour, they may be in a healing coma.
Perform airway opening manoeuvres.
Suction the airway.
- This will help get rid of any secretions/fluid build-ups. All medical areas should have suction machines close at hand (video guide).
If required, insert new airway.
- Oropharyngeal for patients who are unconscious (video guide).
- Nasopharyngeal for patients who are partly or fully conscious. Do not use in patients with potential skull fractures (video guide).
- A tracheostomy may be needed in severe cases (video guide).
Count the respiratory rate.
- Is it too slow? - slow respiratory rate (bradypnoea) causes include sedation or an increase in intracranial pressure caused by trauma or infection.
- Is it too fast? - fast respiratory rate (tachypnoea) causes include an airway obstruction, a virus, heart(s) failure, or a recent regeneration.
Observe for respiratory distress.
- Are they turning purple? - indicates poor circulation or damage to the respiratory system.
- Are they using their abdominal muscles excessively to breathe? Is their chest falling particularly deeply? Are they unable to speak in full sentences?
- Is the breathing not equal on both sides of the chest? - this could indicate a pneumothorax.
- Are they coughing? - if it's productive (produces mucus/sputum) this could indicate an infection such as pneumonia. If it's not productive (a 'dry' cough) this could be caused by asthma or lung scarring.
Listen to their breath.
- Is it rattling? Are they wheezing? Is it high-pitched (stridor)? - they may have a partial airway obstruction.
- Is it extremely irregular (Cheyne-Stokes respiration)? - this could be due to stroke or heart(s) failure.
- Is it deep and sighing (Kussmaul's respiration)? - they may be experiencing diabetic ketoacidosis.
Assess tracheal position.
- The trachea should be central. Warning: examining it can be uncomfortable for a conscious/semi-conscious patient.
- The trachea will deviate away from a tension pneumothorax.
Tap (percuss) their chest (video guide).
- The sound should resonate. A dull sound could indicate a tumour or partial collapse of the lung, while a hyper resonance could indicate a pneumothorax.
Listen to (auscultate) their lungs.
🚫
Human technology can't detect the amount of oxygen in a Gallifreyan as oxygen doesn't travel in their blood, so pulse oximeters don't work and cannot give an SpO2 reading.
🚫
A human doctor might be tempted to order an arterial blood gas (ABG) test, however, as above oxygen doesn't travel in the blood, so an ABG will give you nothing.
Do a chest scan.
Administer oxygen.
- Typically using a mask with an oxygen flow rate of 15L.
Sit the patient upright if able.
- This will help aid breathing.
Other pathology.
- During the assessment, if any other conditions were identified they should be managed appropriately.
Perform a general visual assessment.
- What colour is their skin? - being pale could suggest anaemia or partial heart(s) failure.
- Are they swollen? - a swollen face points towards anaphylaxis, while swollen limbs suggest heart(s) failure.
- How are their veins? - if they're shrunken and colourless, this points to severe blood loss, circulatory issues or hearts(s) failure. If the jugular is raised, this is a red flag for heart(s) failure.
Check their extremities.
- Temperature - are their hands symmetrically warm? Cold hands could indicate heart(s) failure. If one hand is colder than the other, this could suggest circulatory problems.
- Skin presentation - are their hands discoloured or mottled? This could suggest circulatory problems.
- Capillary refill time - put pressure on a fingertip for long enough for the skin to blanch, then let go. How long does it take to return to normal colour? - It should be under 1 second. Anything longer can indicate circulatory problems.
Listen to their hearts.
Check their heartsrate.
- Is it too slow? - slow heartsrate (bradycardia) causes include heart/s failure, or drugs.
- Is it too fast? - fast heartsrate (tachycardia) causes include blood loss, an infection, pain, aspirin poisoning, dehydration, hypoglycaemia, or a recent regeneration.
Check their pulse.
- Check the rhythm and rate - irregular or weak is a red flag that one of their hearts have failed.
Check their blood pressure.
- Too high (hypertension)? - this could be due to a stroke, or too much fluid (hypervolaemia) possibly indicating kidney failure.
- Too low (hypotension)? - this could indicate fluid loss like blood loss (hypovolaemia), sepsis, aspirin poisoning, or a recent regeneration.
Perform a fluid balance assessment.
- If able, get a history of the patient's fluid intake. Is as much going in as it is going out?
- Reduced urine output (oliguria) could point to dehydration or heart(s) failure.
- Increased urine output (polyuria) could indicate diabetes or kidney injury/failure.
⚠️
Keep in mind that a healthy Gallifreyan has a
much lower urine output than humans. A normal output for humans would be considered excessive in Gallifreyans.
⚠️
At this point any good doctor will order blood tests including a Full Blood Count (FBC), a U&E (Urea and electrolytes), or a Liver Function Test (LFT). Keep in mind that Gallifreyan blood is
extremely difficult to interpret.
Order an electrocardiogram (ECG).
- ECG results will be somewhat difficult to interpret due to the second heart. However, it's useful for detecting if the second heart has failed or if one is irregular or weaker than the other (video guide).
Do a bladder scan.
- Bladder scans will show if there's any urinary retention. In Gallifreyans, the scan should be below 50ml. (I can't find a good video guide, but for your info bladder scanners are portable and available, just smear the bladder area with gel, follow the instructions for placement on the machine and pull the trigger clicker to get an instant readout in ml).
Implement fluid monitoring.
- Known as a fluid balance chart, both intake and outtake are monitored by medical staff.
Introduce intravenous fluids/blood.
- This will require a cannula to be placed. Remember Gallifreyan skin is tougher and it may be slightly harder to find a vein and insert it (video guide).
- Once inserted, IV fluids can be introduced if needed at 500ml over 15 minutes. Reassess after 15 minutes and repeat up to four times. If there's any form of heart(s) failure, these figures should be halved.
- If a blood transfusion is required, Gallifreyans can benefit from human blood but their own blood/blood from another Gallifreyan is preferable (video guide).
⚠️
A Gallifreyan MUST receive blood from a member of their House. Any transfusions between Gallifreyans who do not share their House will result in septicaemia.
Consider catheterisation.
- This is used to relieve any urinary retention or create more accurate monitoring of urine output (male and female video guides).
Assess their level of consciousness.
- Alert: Are they awake or partially awake?
- Verbal: Do they respond to your voice?
- Pain: Do they respond to pain?
- Unresponsive: The patient doesn't respond to any of the above.
- If you need to be more detailed in assessing their consciousness level, use the Glasgow Coma Scale (GCS).
Check their neurological function.
Review their medical history.
- Known conditions - do they have any known conditions that could be contributing factors to their current presentation?
- Medication - has anything been administered that could be contributing to their presentation? This could be drugs such as sedatives or opioids.
⚠️
If aspirin or another drug affecting blood (eg. an antiplatelet or antifibrinolytic drug) has been used, suspect anaphylaxis.
Check their blood glucose levels.
- This can be done with a normal finger-prick test, keeping in mind it'll take a bit more force to break the skin, and you'll need to be quick before they clot (video guide).
- Human medics will read the normal Gallifreyan levels as hyperglycaemia. Any attempt to control these levels will cause the Gallifreyan to start breaking down their own fat and fat reserves for energy, resulting in elevated ketone levels. This mimics a diabetic ketoacidosis attack.
- Abnormally low levels could indicate a recent regeneration, starvation, or use of the Detox.
Order a head CT.
- This can reveal damage to the brain which may be affecting neurological functions. The scan is going to be a little complicated to read but should be interpretable.
- For in-depth explanations on interpreting human head CTs, see more.
Glucose management.
- Hypoglycaemia (glucose levels below 6 mmol/L): If patient is conscious, give glucose gel by mouth, repeating up to a further 3 times every 10-15 minutes until normal glucose levels are reached. If unconscious or unable to take orally, administer 250 ml of glucose intravenously. Once patient is alert, provide a long-acting glucose source, like fruit or bread.
Assess their pain level.
- Determine if they're in pain and how much, and follow the intervention section below.
Inspect their skin for abnormalities.
- Rashes - could indicate an infection or drug reaction.
- Bruising - could indicate a trauma or circulatory problems.
- Swelling/discolouration/discharge around IV lines or surgical sites - could indicate an infection.
Check their temperature.
- An abnormally high temperature could indicate an infection.
- An abnormally low temperature could indicate cold exposure or a healing coma.
Take cultures/swabs.
- Take a sample/swab of any apparent infection sites so it can be analysed to check for the infection type.
Manage pain levels.
- Mild pain - use a non-opioid eg. paracetamol (2g every 4-6 hours).
- Moderate pain - use a weak opioid in conjunction with the above eg. codeine (60-120mg every 4-6 hours), tramadol (100-200mg every 6 hours).
- Major pain - withdraw the weak opioid and replace with a strong opioid eg. morphine (10-20mg every 4 hours or as needed).
🚫
In no case should aspirin ever be considered for pain management as this will cause a severe allergic reaction in a Gallifreyan possibly leading to coma and death/regeneration.
Start antibiotics if severely unwell.
- Most antibiotics will work on Gallifreyans. Drugs will differ depending on the infection type, and remember it's double the standard dosage for them.
Resources